Zainab Shafique, Bushra Kiran, Fatima Zahra Naqvi, Muhammad Arif Zafar, Riaz Hussain Pasha, Muhammad Akram Khan & Muhammad Farhan Rahim
Veterinary Phytotherapy: Exploring the Use of Plants in Animal Health and Treatment
SUMMARY
The use of plants for healing, known as phytomedicine, has ancient roots, and one famous plant in this tradition is Chlorophytum (C.) borivilianum. This plant, also called Musli or Safed Musli (Urdu), is used extensively in traditional medicine and Ayurveda. C. borivilianum, has been recognized for its aphrodisiac, immune-modulatory, and antioxidant qualities and is rich in active ingredients such as proteins, polysaccharides, and saponins. Its potential applications in the treatment of ulcers, bacterial infections, and cancer have been highlighted by recent studies. It has antioxidant properties and also the ability to address male infertility. This herb has immune-modulating, reproductive health, and fertility-enhancing properties. Furthermore, it helps to alleviate menstrual symptoms and improve physical features such as vaginal lubrication and drying. It plays a role in areas such as longevity of reproduction, hormonal balancing, and general health. Care should be taken regarding its dosage because it can result in allergic reactions or hormonal imbalances in case of overdose. Due to its ability to improve uterine receptivity, regulate the mensural cycle, and enhance sperm and egg quality, C. borivilianum may have ART applications. It has wide economic importance in both international and local markets. In order to improve reproductive health and for patients who are unable to conceive, C. borivilianum offers an effective and natural alternative to conventional reproductive treatment.
- Department of Clinical Studies
- Department of Veterinary Biomedical Sciences
- Department of Pathology
- Faculty of Veterinary and Animal Sciences
- Pir Mehr Ali Shah-Arid Agriculture University, Rawalpindi, Pakistan.
- *Corresponding author: dr.mazafar@uaar.edu.pk
INTRODUCTION
The World Health Organization
IMPACT OF GESTATIONAL MATERNAL UNDERNUTRITION ON FETAL DEVELOPMENT
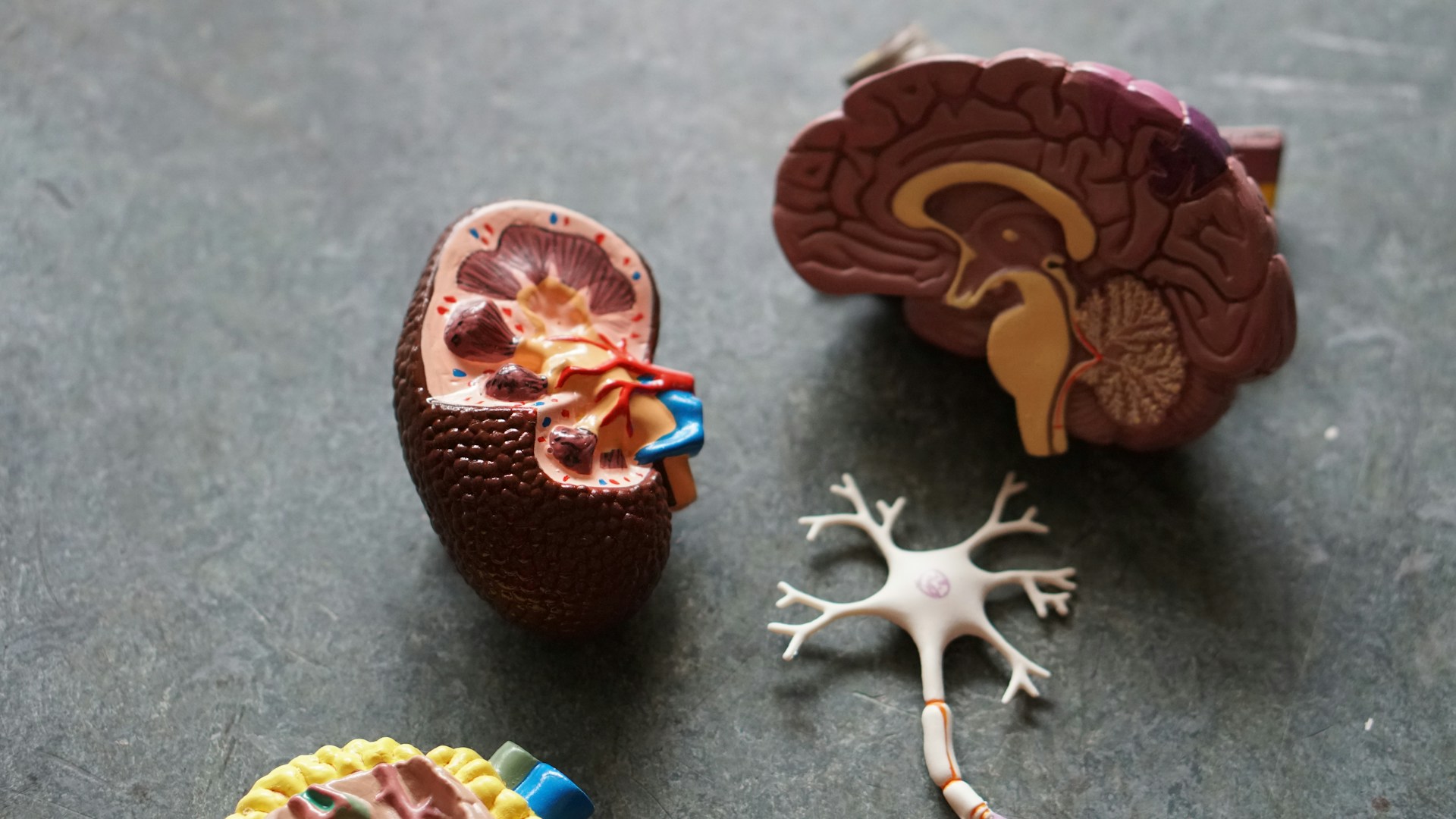
Maternal undernutrition has been proven to have a profound effect on fetal growth, with body weight and many key organs. It has been reported previously that during the first two weeks of pregnancy, the provision of a 5% protein diet only (undernutrition) led to a reduction in brain weight, size, and cortical thickness of the brain (Gressens et al., 1997). A severe gestational maternal protein restriction in rats caused a reduced number of glomeruli and hypertension in both male and female newborns, this hypertension is salt-sensitive and worsens with age, but is approximately equivalent in males and females (Woods et al., 2004)
Chronic energy deficit or maternal undernutrition means
having a body mass index (BMI) below 18.5. If the females are
under-nourished females at the time of conception, then during
pregnancy (when there are additional demands due to the
growing fetus), they are unlikely to improve their nutritional
status. They are more likely to fail to gain sufficient weight
during pregnancy and are at a higher risk of mortality than wellnourished and healthy women (Smith et al., 2003).
IUGR predisposes developing fetuses to reduced organ and
body weights. Most information about the long-term and short term effects of IUGR has come from animal models. In recent
years, many animal models of placental insufficiency and/or
poor maternal nutrition have been developed to investigate the
causes and effects of IUGR. Both maternal dietary
manipulations and surgical interventions have been employed
for these studies. A number of animal species have been studied
for IUGR effects, including rodents, rabbits sheep, and primates
(Louey et al., 2000; Mitchell et al., 2004; Jonker et al., 2018).


What to read next...
Sulaiman Khan, Riaz Hussain Pasha, Iqra Ali, Awais ur Rehman Sial, Ayesha Humayun, Adnan Hassan Tahir & Muhammad Arif Zafar
Hassnain Khan, Muzammil Zaman Khan, Mayra Ihsan, Nizam-Ud-Din1, Azka Zaheer, Bilal Ahmed Khan, Aneela Gul & Jameel Ahmed Buzdar
Evelyn Saba, Mansur Abdullah Sandhu, Arfan Yousaf, Usman Rashid & Man Hee Rhee