Sana Asif, Lariab Saeed, Talha Umar, Muhammad Umar, Huili Feng, Talha Adil, Aftab Ali Khan & Saqib Umer
Chlorophytum borivilianum (Musli): A Promising Alternative to Conventional Reproductive Treatment
SUMMARY
- Department of Theriogenology, University of Agriculture, Faisalabad-38040, Punjab, Pakistan.
- Department of Clinical Veterinary Medicine, College of Veterinary Medicine, Huazhong Agricultural University, Wuhan-430070, PR China.
- Authors contributed equally
- Corresponding author: saqib.umer@uaf.edu.pk
INTRODUCTION
Phytomedicine is the use of plants to cure illness or prevent disease, a practice that has been around for generations. Herbs may be utilized as an alternative to or in conjunction with conventional treatment, so there’s no need to disregard the former. Research into alternative medical practices, such as phytomedicine or ethnomedicine, is not new. For the first time in the 1960s, Tabebuia (T.) impetiginosa (Red Lapacho) drew significant attention as a ‘wonder medicine’ in Brazil and Argentina. T. impetiginos has two major bioactive components: lapachol and betalapachone. The principal antitumor component is beta-lapachone, and pro-apoptotic actions were identified in vitro. An endangered geophyte with extensive traditional use and therapeutic value is Chlorophytum (C.) borivilianum (Liliaceae). C. borivilianum (Hindi for “white tubers”) is the prevalent name for this food item. The root of the C. borivilianum plant is given a prominent position in the Ayurveda, Unani, Homeopathic, and Allopathic medical traditions. Traditional C. borivilianum usage has been mostly unreported since they have been conveyed orally from one generation to the next in local spoken languages. Recent surveys in various Indian states have shown that the ethnic communities of the Aravali Hills (Meena), Rajasthan (Mizo), Mizorum (Mizo), Maharashtra (Pawra and Thakar), and Madhya Pradesh (Korku and Bharia) have benefited from safed musli’s inclusion in their health care system, increasing their health, vitality, and longevity as shown in Fig 1., ( Patil, 2003; Meena & Rao 2010; Deshwal & Trivedi 2011; Rai & Lalramnghinglova 2011).
The World Health Organization
IMPACT OF GESTATIONAL MATERNAL UNDERNUTRITION ON FETAL DEVELOPMENT
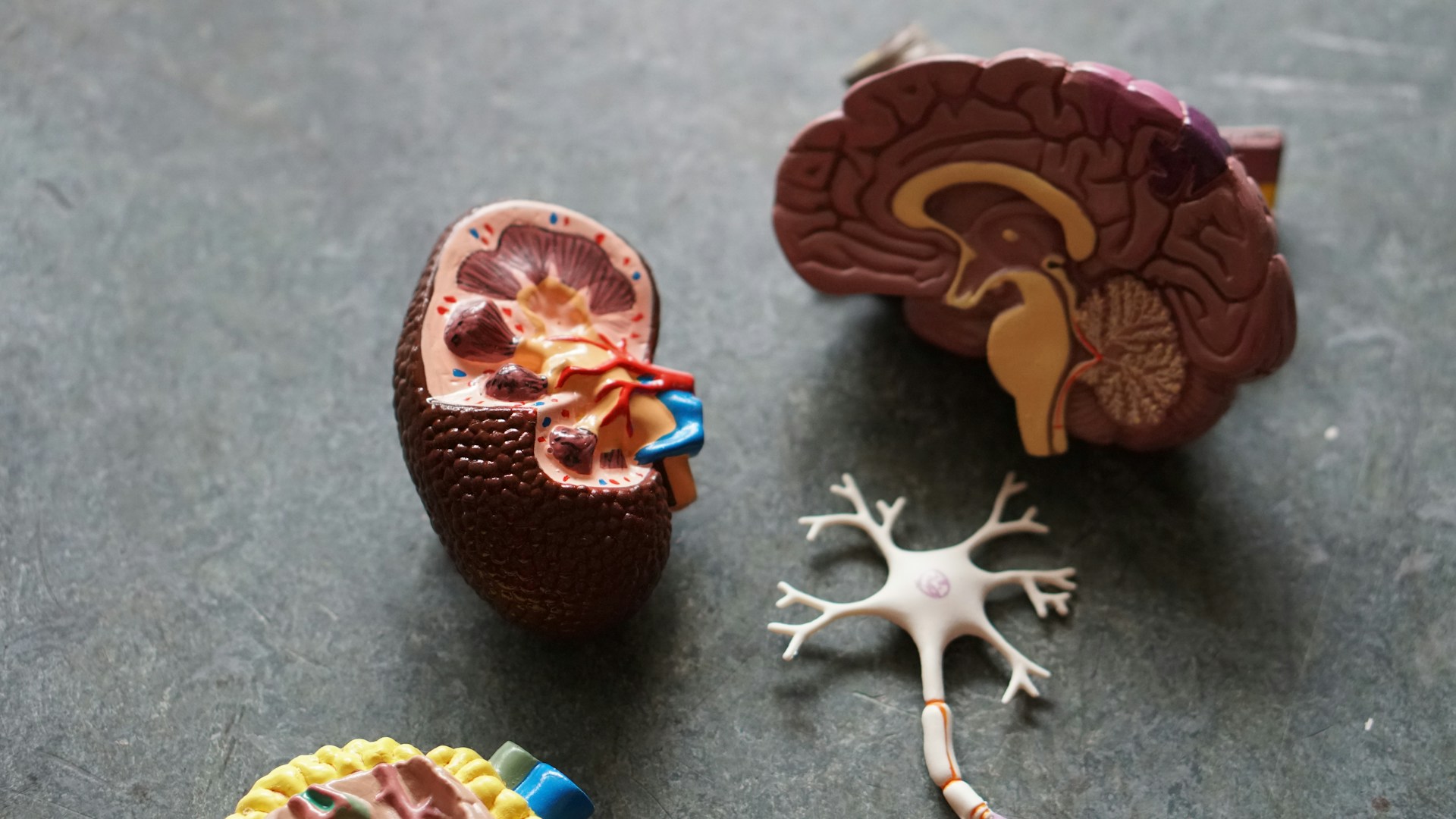
Maternal undernutrition has been proven to have a profound effect on fetal growth, with body weight and many key organs. It has been reported previously that during the first two weeks of pregnancy, the provision of a 5% protein diet only (undernutrition) led to a reduction in brain weight, size, and cortical thickness of the brain (Gressens et al., 1997). A severe gestational maternal protein restriction in rats caused a reduced number of glomeruli and hypertension in both male and female newborns, this hypertension is salt-sensitive and worsens with age, but is approximately equivalent in males and females (Woods et al., 2004)
Chronic energy deficit or maternal undernutrition means
having a body mass index (BMI) below 18.5. If the females are
under-nourished females at the time of conception, then during
pregnancy (when there are additional demands due to the
growing fetus), they are unlikely to improve their nutritional
status. They are more likely to fail to gain sufficient weight
during pregnancy and are at a higher risk of mortality than wellnourished and healthy women (Smith et al., 2003).
IUGR predisposes developing fetuses to reduced organ and
body weights. Most information about the long-term and short term effects of IUGR has come from animal models. In recent
years, many animal models of placental insufficiency and/or
poor maternal nutrition have been developed to investigate the
causes and effects of IUGR. Both maternal dietary
manipulations and surgical interventions have been employed
for these studies. A number of animal species have been studied
for IUGR effects, including rodents, rabbits sheep, and primates
(Louey et al., 2000; Mitchell et al., 2004; Jonker et al., 2018).


What to read next...
Sulaiman Khan, Riaz Hussain Pasha, Iqra Ali, Awais ur Rehman Sial, Ayesha Humayun, Adnan Hassan Tahir & Muhammad Arif Zafar
Hassnain Khan, Muzammil Zaman Khan, Mayra Ihsan, Nizam-Ud-Din1, Azka Zaheer, Bilal Ahmed Khan, Aneela Gul & Jameel Ahmed Buzdar
Evelyn Saba, Mansur Abdullah Sandhu, Arfan Yousaf, Usman Rashid & Man Hee Rhee